A new type of genetically engineered T-cell therapy has been developed by researchers at the Peter MacCallum Cancer Centre that could effectively eliminate solid cancer tumors.
The innovative approach uses stem-like T-cells instead of conventional T-cells, which have shown an increased ability to reproduce when carrying the chimeric antigen receptor (CAR) receptor.
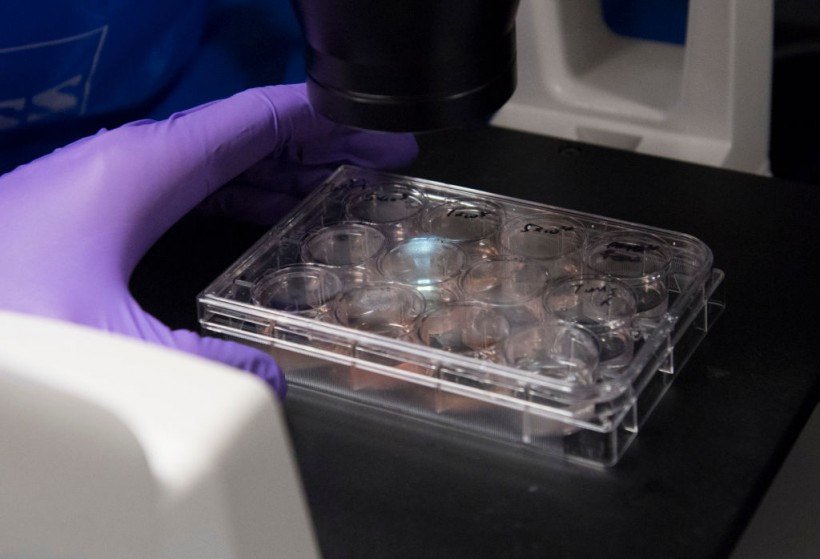
Dr. Benjamin Jin, a biologist working on immunotherapy for HPV+ cancers, works in the lab of Dr. Christian Hinrichs, an investigator at the National Cancer Institute at the National Institutes of Health (NIH) in Bethesda, Maryland, February 7, 2018. - Experimental trials are ongoing at the National Institutes of Health Clinical Center. In this US government-funded research hospital, doctors are trying to partially replace patients' immune systems with T-cells that would specifically attack cancers caused by the human papillomavirus (HPV), a common sexually transmitted infection.
CAR T-cell Therapy
CAR T-cell therapy is an innovative form of immunotherapy that utilizes naturally occurring T-cells, a crucial part of the body's immune system, to target and destroy infected cells.
These T-cells are harvested, re-engineered with the CAR receptor, and then re-infused as a one-time procedure to fight cancer cells.
The new Peter Mac-led study uses stem-like T-cells instead of conventional T-cells. These cells, known as T stem-like CAR T-cells, have demonstrated an increased ability to reproduce when carrying the CAR receptor, indicating they may be more effective in eliminating cancer cells.
According to Professor Paul Neeson, head of the Human Immunology Translational Lab at Peter Mac, this study is a significant step toward CAR T-cell therapy being effective in solid cancers.
"While CAR T-cell therapy has been approved in some types of blood cancers like leukemia, lymphoma, and myeloma, the success of CAR T-cells in solid cancers is limited. This is due to factors such as poor CAR T-cell expansion, persistence, and exhaustion when fighting the tumor," he said in a statement.
He added that these T stem-like CAR T-cells have improved anti-tumor function in the culture dish and four pre-clinical models. They have even eradicated pre-existing solid tumors combined with the immune checkpoint drug anti-PD1.
Read Also: Exhausted Cancer-Fighting T Cells Can be Reinvigorated to Protect the Immune System, New Study Finds
Production Protocol
The study first developed a production protocol that produces fully functional stem-like CAR T-cells in a condensed six-day time frame rather than the usual 14 days, paving the way for a future process that could be more efficient and scalable.
These findings encourage the utilization of manufacturing techniques to create stem-like CAR T cells for clinical applications.
These cells would be used to treat two unresponsive pediatric leukemias to current therapies. According to Prof. Neeson, they are certain that their process can harmonize the CAR T-cell product into one with reliable anti-tumor activity and the crucial capacity to endure.
Once the researchers have established the safety of these cells, they will focus on creating this treatment for solid pediatric malignancies, including osteosarcoma and neuroblastoma.
The Murdoch Children's Research Institute, Zero Childhood Cancers, Children's Cancer Institute Australia, and several doctors at Peter Mac all collaborated in the study.
The researchers believe that the new production protocol could make the treatment more affordable and accessible to patients in the future.
Related Article: Magnetic Nanoparticles To Prevent Lung Cancer! Triggering Anti-Cancer MicroRNA! Efficiency, Safety, and Other Details