Excessive insulin can be just as deadly as a lack of insulin, according to a new study.
However, there is also good news as researchers at the University of California San Diego School of Medicine discovered that the body has a natural defense mechanism against too much insulin.
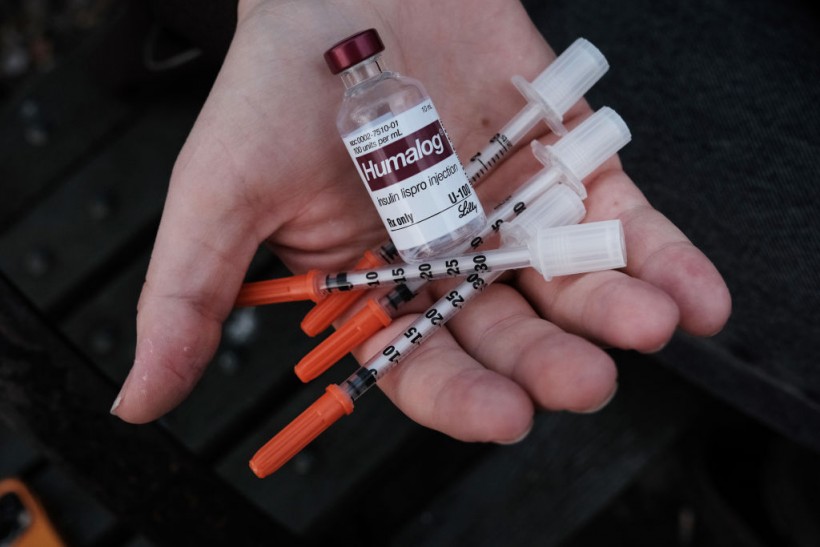
NEW YORK, NEW YORK - MARCH 02: In this photo illustration, Taylor Jane Stimmler, whose had type 1 diabetes since she was a teenager, displays her insulin and needles used for injection on March 02, 2023, in New York City. Drugmaker Eli Lilly announced yesterday that it would cap the out-of-pocket cost of its insulin at $35 a month. Medical experts believe that the unexpected move may compel other insulin makers in the U.S. to follow suit and cap their prices on insulin.
"Safety Valve"
The metabolic enzyme fructose-1,6-bisphosphate phosphatase (FBP1) acts as a "safety valve" to prevent insulin shock, a condition that can lead to seizures, coma, and even death if left untreated.
Insulin is a crucial hormone that is necessary for the treatment of type 1 and type 2 diabetes, with approximately 8.4 million Americans relying on insulin therapy, according to the American Diabetes Association.
The latest study sheds light on how the body regulates insulin production to maintain balance. However, insulin or insulin-stimulating medications can disrupt this process, causing hypoglycemia, or low blood sugar, which is a leading cause of death in individuals with diabetes.
The research team, led by senior study author Michael Karin, Ph.D., found that FBP1 plays a critical role in controlling gluconeogenesis, a process in which the liver produces glucose during sleep and releases it into the bloodstream for energy.
In addition, FBP1 inhibits the primary pathway of insulin activity, protein kinase AKT. Insulin hyper-responsiveness can occur without FBP1, leading to hypoglycemic shock and acute fatty liver disease.
Developing a Mouse Model
The researchers developed a mouse model with liver-specific FBP1 deficiency that accurately replicated the human condition.
The mice showed no symptoms of illness until they were fasted, which resulted in severe hypoglycemia and liver abnormalities.
The study also found that a combination of FBP1 deficiency and glucose starvation led to other negative effects such as an enlarged, fatty liver, mild liver damage, and elevated blood fats.
To better comprehend FBP1's functions, they created a peptide derived from FBP1 called E7. E7 disrupted the association between FBP1 and AKT and another protein that inactivates AKT.
E7 acts like an insulin mimetic by activating AKT. In mice with insulin resistance due to a high-fat diet, injecting E7 reversed the resistance and restored normal blood sugar control.
The researchers aim to develop E7 further as a viable alternative to insulin treatment. Unlike insulin, E7 is unlikely to cause insulin shock, which can be deadly.
The findings of the study reveal more information about the body's natural defenses against excessive insulin and the crucial role of FBP1 in preventing insulin shock.
The research team's findings were published in the journal Cell Metabolism.
Related Article: This Wearable Artificial Pancreas Device Helps Track Blood Glucose and Add Insulin-Here's How It Works